Contact was made shortly after dawn on 26 June 2008 by the Marine Special Operations unit as it entered a narrow valley in far western Afghanistan. A routine reconnaissance patrol was ambushed. A fierce firefight resulted as the insurgents directed accurate small arms fire down from positions on the canyon walls. The American Marines and their Afghan allies dismounted to return fire. In the ensuing melee, one Marine was killed and six others were wounded. The patrol’s two Navy corpsmen were among the casualties. A request for casualty evacuation to the Marine Special Operations Command (MARSOC) operations center at Farah triggered an immediate response. This action would confirm the validity of the Special Operations Resuscitation Team (SORT) from the 528th Sustainment Brigade (A).


Army Staff Sergeant (SSG) Michael R. Fulghum and SSG Antujuan Brown, the two Special Operations Combat Medics (SOCMs) on the SORT, grabbed M-9 medical bags and ran out to board two UH-60 Black Hawk helicopters on the Forward Operating Base (FOB) helipad. “SSG Brown got on the MEDEVAC [medical evacuation] bird and I jumped on the chase bird [an armed UH-60] and we took off,” said SSG Fulghum. “It was a twenty minute flight out there but we circled for an hour while the Marines tried to break contact and withdraw so we could get them.”1
While Close Air Support (CAS) aircraft dropped 500-pound bombs on the enemy positions, the Marines managed to break free from the ambush. The two Black Hawks alternately swooped down to pick up wounded Marines and Afghan soldiers; three casualties per helicopter. None of the casualties were on litters. To his horror, SSG Fulghum realized that one of his patients, a badly wounded Navy Corpsmen, was a friend.

“’Tony’ had been shot through the left side and had a gaping wound in his lower chest wall,” said Fulghum. “His intestines were coming out and he was bleeding badly. It was chaos inside the aircraft. As the helicopter took off, two open bandages blew out the window. I got an IV in him and a dressing on the wound, but it was real bad.”2 As the two Black Hawks raced back to Farah, Fulghum checked the other two casualties.

“The Afghan was shot in the upper arm, but not too bad. The wounded Marine was hit in the upper thigh and had two tourniquets on his leg. He was still bleeding steadily so I put another tourniquet on above the others. It wasn’t much help, but I had to get back to Tony. That fifteen minute flight seemed like an eternity,” SSG Fulghum recalled.3 When the helicopters touched down, the patients were off-loaded onto litters and rushed into the small FOB hospital. The helicopters took off to bring back three more casualties.
“As the helicopter took off, two open bandages blew out the window. I got an IV in him and a dressing on the wound, but it was real bad.” — SSG Michael R. Fulghum
For the next thirty-six hours, SORT personnel worked nonstop to stabilize the nine casualties sufficiently to evacuate them to the Army combat support hospital at Bagram. Everyone survived. The lifesaving that took place on 26 June 2008 validated the SORT concept for Army SOF as well as the team’s pre-mission training. This article will explain the mission preparation and how the SORT supported the Combined Joint Special Operations Task Force-Afghanistan (CJSOTF-A).
The SORT was created by the 528th Sustainment Brigade, Special Operations (Airborne) (Provisional) at Fort Bragg, North Carolina, to provide the stabilization and evacuation of casualties in Army Special Operations Forces (ARSOF) units and to reduce the patient administrative burden on unit medics. ARSOF needed a small, highly responsive lifesaving/life preserving medical organization that was leaner and more agile than that provided by the U.S. Army Medical Corps. Normally an 80-man Area Support Medical Company (ASMC), operating a small field hospital has this responsibility. The ASMC has a 40-bed holding capacity, provides ground ambulance evacuation, laboratory, X-ray, dental, and patient administration services for a corps area.4 The 8-man SORT, reinforced by a small surgical team and dedicated air evacuation capability, was designed to provide Advanced Trauma Management (ATM) to ARSOF units in remote field locations. This was the mission to be validated by the first SORT deployed by the 528th.5
Captain (CPT) Jamie C. Riesberg, MD, the physician on the team, was an original member of the organization. After finishing his residency in Family Medicine at Womack Army Hospital, Fort Bragg in 2006, he was assigned to the battalion surgeon’s office of the Special Operations Sustainment Brigade. “The SORT grew out of the Special Operations Medical Association Conference in Tampa in 2004,” said Riesberg. “The problem was how to provide Role II [second echelon, resuscitation and stabilization] medical support to ARSOF. The Army medical organization had too big a footprint. LTC Lorykay Wheeler, the 528th surgeon, built the capability that became the SORT.”6 The team structure reflected their mission of managing trauma on the battlefield.

“Based on our first OIF experience in 2003, it was clear that the SOSCOM [Special Operations Support Command] was not able to provide the second echelon of medical support that the ARSOF units needed when they first entered theater,” said LTC Lorykay W. Wheeler. “ARSOF has always depended upon conventional Army medical units to provide the Role II medical care. When we went to Iraq in 2003, the medical units that were programmed to support us took quite a while to flow in. Eventually a Forward Surgical Team [FST] showed up, but we needed their capability at the beginning.”7 After her tour in Iraq, LTC Wheeler worked with the surgeons of U.S. Army Special Operations Command (USASOC) and United States Special Operations Command (USSOCOM) to create a small, deployable organization that would fill the gap between the ARSOF team medics (Role I) and the U.S. Army Medical Corps Role II medical support.
“The SORT was originally created as an expeditionary, short-term fix until the theater medical assets were established,” said Wheeler. “It was designed to operate in an austere environment like we have in Afghanistan, where the coverage is difficult to provide due to the great distances and lack of Role II facilities.”8 The SORT concept survived the ARSOF logistical support reorganization that eliminated the 528th Special Operations Support Battalion.

“In putting together the TDA [Table of Distribution and Allowances], we had to take into account that the Special Forces PAs [Physician’s Assistants] and medical teams had gone to the GSBs [Special Forces Group Support Battalions] when the 528th Battalion was disbanded in 2005,” said CPT Riesberg. “By TDA, the SORT had a physician with Emergency Room or Family Medicine training, a Registered Nurse [RN] with emergency medicine or critical care experience, two SOCMs, a Licensed Practical Nurse [LPN], one X-ray technician, one laboratory technician, and one patient administration specialist.”9 The team did not have all these personnel for the 2008 Afghanistan mission.
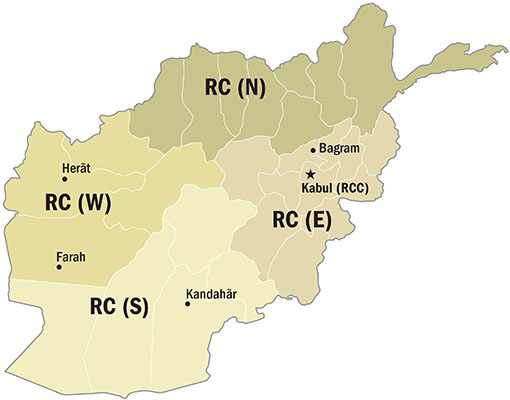
The SORT supported the 7th Special Forces Group (7th SFG) from April to December 2008. The 7th SFG staff formed the nucleus of Combined Joint Special Operations Task Force-Afghanistan (CJSOTF-A), which controlled Coalition special operations forces throughout the country. It was a multi-national and multi-service organization. The 7th SFG surgeon, LTC Andrew L. Landers, was dual-hatted as the CJSOTF surgeon.
“I requested the SORT because we needed a scaled-down package to provide their Role II [medical and surgical] capability in Farah,” said Landers. “The operating environment there was austere and the distances for evacuation were long.”10 Farah was a four-hour flight from Bagram on the other side of the country. “The SORT gave us an agile capability that we could move as necessary,” said LTC Landers. “They provided the ability to stabilize casualties and, if necessary, their people could accompany the patient during the evacuation to the next level of care. They did that several times.”11 The initial SORT mission was to support the MARSOC forces in Farah, in extreme western Afghanistan. Having been alerted for deployment, the team conducted an intensive pre-mission training program.

Riesberg was the team physician. CPT E. Edward Dunton, RN, was the SORT Team Leader. SSG Brian P. Moore, one of two X-Ray technicians, served as the Team Sergeant. SSG Michael R. Fulghum and SSG Antujuan Brown were the two SOCMs. Specialists (SPC) Donnell B. Smith, an X-ray technician, Ronnie M. Heflin, a laboratory technician, and Dwayne A. Bostic, a patient administration specialist, rounded out the team. There would be no PA or LPN. Cross-training provided medical specialty redundancy. The team trained to cover their requirements for communications, supply, and maintenance. Surgical support was to come from in-country Army medical assets.
“We had to make sure everyone was cross-trained,” said SSG Brian P. Moore. “We were starting from a blank slate. We had to do weapons qualification, survival training, and our MOS [military occupation specialty] training to get ready. We had about a month and a half when we got the word for the deployment.”12 After one false alarm, the team got the deployment orders in February 2008.
“Originally 3rd Special Forces Group requested us for Afghanistan in October 2007,” said CPT Ed Dunton. “That got turned off in February 2008. 7th Group requested us when they took over the CJSOTF mission from 3rd. When we first got the word that we were going with 7th [SFG], we did not have an exact [operational] location. Consequently we loaded all our tentage, water purification systems, generators, and everything in three ISU-90 containers.”13 The SORT left Pope Air Force Base with all its equipment on 21 April 2008 aboard a C-17 Globemaster III. After stopping briefly to refuel at Spangdalem Air Base in Germany, they arrived at Bagram, Afghanistan, on 22 April.
The SORT remained at Camp Vance, in Bagram for ten days. During that time they secured additional supplies and coordinated procedures with the theater hospital for the reception of patients. The 3rd SFG handed off the CJSOTF mission to the 7th SFG on 1 June 2008. The CJSOTF surgeon, LTC Andrew L. Landers, wanted the SORT to cover operations in RC-West.
“I was able to meet with the team prior to their deployment,” said LTC Landers. “I told them their goal was to ensure that anyone who was alive when they were received by the SORT would remain alive as long as they were under the team’s control and were handed off to the next higher level of medical care.”14 Landers reminded the team not to forget their primary mission.
“I told them their goal was to ensure that anyone who was alive when they were received by the SORT would remain alive as long as they were under the team’s control and were handed off to the next higher level of medical care.” — LTC Landers
“His guidance to me was pretty straight forward,” said CPT Ed Dunton. “Do not degrade your capability.”15 The mission for the SORT was to support the MARSOC element and all coalition units operating in Regional Command-West (RC-West). A city of roughly 40,000 inhabitants, Farah was the primary urban center in the region. An Afghan district hospital was there.
Less than a mile out of Farah, the team found three small, closely-spaced compounds. There was an airfield that could handle large transport aircraft. The compounds and the airfield were enclosed by a concertina wire perimeter fence. The first compound, where the SORT billeted, was occupied by two Marine special operations teams, (thirty-five Marines), from Hotel Company, 2nd Marine Special Operations Battalion (2MSOB). Adjoining the MARSOC compound was a second base used by the Afghan National Army (ANA). It held an ANA infantry company (less than 100 personnel) and their 25-man U.S. Army Embedded Training Team (ETT) made up of active Army and National Guard advisors. The ANA company was part of the 3rd Kandak (Battalion), 1st Brigade of the 207th Corps. The rest of the 3rd Kandak was based in Farah. Inside the ANA compound was a small four-man CJSOTF Civil Affairs team whose mission was to distribute humanitarian assistance funds and supplies.16



Three hundred yards from the Marine compound was the American Provincial Reconstruction Team (PRT) base. Sponsored by the various Coalition nations, the PRT is a multi-service organization with military and civilian personnel. Their mission is to facilitate humanitarian relief and reconstruction.17 Among the more than one hundred personnel in the PRT was a medical team of U.S. Navy Reservists with two physicians, a PA, a laboratory technician, and two corpsmen. The PRT base also housed the surgical team from Task Force-Med (TF-Med) from the U.S. Army theater medical organization. The TF-Med team had been in Farah for six months. The team was made up of U.S. Army Reserve personnel and had a general surgeon, a nurse-anesthetist, two operating room technicians, an intensive care nurse, an LPN, and two medics. They provided the surgical capability the SORT did not have.18 Now three medical teams would operate out of the ten-room hospital on the PRT compound.

The medical facilities, while better than expected, were quite small and austere by U.S. standards. The largest room in the hospital was the four-bed trauma ward for incoming patients. There was an operating room, a pair of intensive care holding areas for patients coming out of surgery with two beds each, and an intermediate holding area with two beds for stabilized patients awaiting evacuation. The hospital had a pharmacy, a central supply room that doubled as the area for sterilizing the surgical equipment, a small laboratory, a room where the SORT set up their communications equipment, and a break room.19 The air-conditioned building had a dedicated generator and an emergency back-up system. Space was at a premium so the SORT medical supplies were stored in 40-foot MILVAN containers adjacent to the building. With three different medical teams using the same facility, a mutually acceptable routine and standing operating procedures (SOPs) had to be established.
“Initially we had three chains of command,” said CPT Ed Dunton. “Our mission was trauma. The PRT medical personnel took care of their routine sick call as well as the locals and the TF-Med guys did surgery.”20 To reduce confusion in the trauma ward, the SORT demonstrated their well-practiced system. “At first, the guys had different ways of setting up the equipment for each bed,” said SSG Brian Moore. “I set up one bed the way we do it, with everything in a certain spot. The other teams agreed it was a good method and we set up all four that way.”21 That done, the SORT quickly fell into a daily routine; one that kept every member professionally busy in their specialty and with their additional duties.
SPC Donnell B. Smith was the primary X-ray technician on the team because SSG Moore filled the role of Team Sergeant and LPN. “Every patient we received had a chest X-ray, as a minimum. If the doctors needed other shots, I took them there at bedside,” said Smith. “My system is portable. I roll it up to the bedside and shoot it there. The X-ray is digital and can be read on my laptop. I store each patient in a separate [computer] file and the doctors can call up whom they want to see.”22 If more than one patient arrived at once, the small trauma ward got very busy.









